After the CMS announced MACRA’s brand new quality reporting program—Quality Payment Program (QPP)—physicians across the country took a conscious effort in embracing the new rules. The final rule proposes changes that will have a major impact on providers and propel the healthcare industry into the future.
The payment system now steers away from an incentive-based volume reporting to the one that rewards value i.e. based on performance. CMS created the Advanced Alternative Payment Models (APM) and Merit-Based Incentive Payment System (MIPS) related requirements within the QPP Program, mainly to focus more on patient-centered care. The payment system’s patient engagement strategies will not only drive providers to attain a high score and receive incentives; but also, a more predictable Medicare payment schedule can be expected.
Let’s understand what the MACRA’s final rule entails:
The final rule proposed for MACRA (Medicare Access & CHIP Reauthorization Act of 2015) allows participants to choose between two payment tracks of
Medicare:
1. The Merit-Based Incentive Payment System (MIPS)
This method ensures single submission for all providers. The incentive programs presently under Medicare Part B are:
- Physician Quality Reporting System (PQRS)
- Physician Value-based Payment Modifier (VM)
- Medicare Electronic Health Record (EHR)
- Incentive Program for Eligible Professionals (EPs)
Since the providers are required to report separately for each program, these programs have been merged under QPP (MIPS), to reduce the burden of participation.
2. Advanced Alternative Payment Models (APMs)
The APMs payment track enables providers to earn added incentive payments and provides high-quality and cost-efficient care to patients. APMs can apply to a specific clinical condition, a care episode or a population.
A qualified APM is any one of the following:
- A Medicare Shared Savings Program Accountable Care Organization;
- A model expanded under the Center for Medicare & Medicaid Innovation (CMMI) which is not a Health Care Innovation Award recipient;
- Medicare Health Care Quality Demonstration Program or Medicare Acute Care Episode Demonstration Program; or
- A demonstration program required by federal law
Who is impacted?
The QPP program impacts clinicians that also include those with small and solo practices and healthcare IT vendors which include data submission vendors, registries, electronic health records (EHRs) etc.
The QPP timeline: understanding the phased approach of the QPP

A quick summary: changes in the final rule
- Timeline
> Since special policies have been established for the first year of the QPP, the CMS now terms 2017 as a transition year
> The reporting period for participants is a minimum of 90 days and not one year
- Performance based scoring calculation
> The CMS has set the weightage for the performance categories for the transition year (2017):
- Quality performance category score is now 60%
- Advancing Care Information (ACI) performance category score has been set to 25%
- Clinical Practice Improvement Category (CPIA), renamed to Improvement Activities, is 15%
- Resource Use, renamed to Cost performance category, is 0% and will ease the burden on Composite Performance Score (CPS) calculation
> CMS has reduced the performance feedback from 40 episode-based measures to 10 for the transition year, and advises that weightage may gradually increase over the years
> Performance threshold has been set to three points (one point for each performance category i.e. Quality, ACI and Improvement Activities)
> Additional 10% bonus score will be provided if clinicians complete Improvement Activities through their EHRs and provide reporting to public health and clinical data registries
> Negative payment adjustment
- Participants should report at least one quality measure, one improvement activity or a minimum of five required measures in Advancing Care Information Performance category (ACI)
When to start and what’s the impact?
If the individuals are ready, they can begin January 1, 2017 and start collecting performance data or else choose any continuous 90 days between January 1, 2017 and October 2, 2017. Some of the pointers on participation:
Non-participants
If 2017 data is not submitted by March 2018, the non-participants receive a negative 4% payment/adjustment
Submission of minimum data
If participants submit minimum data, for example, one quality measure and one improvement activity from Clinical Practice Improvement Activities (CPIA), they avoid downward payment/ adjustment
Submission of partial-year data
If data of 2017 (at least 90 days) is submitted, participants can earn neutral or positive payment/ adjustment
Submission of full-year data
If full year data of 2017 is submitted, participants earn a moderate positive adjustment
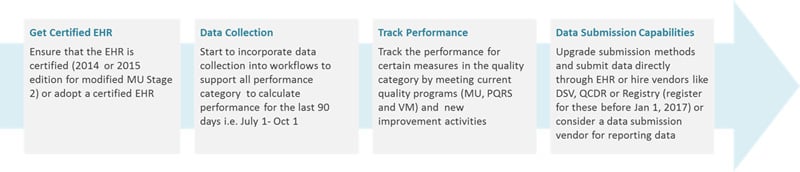
Steps to participate
The clinicians/ vendors who are eager to participate in the Quality Payment Program should start preparing for it early on, to make the most of the special transition-year policies:
Deriving maximum benefits from MACRA
CMS’s goal is to guide the healthcare industry in a direction which focuses on quality and propels them to utilize technology in a bid to improve patient outcomes.
APMs and MIPS are payment tracks which have been designed for a greater inclusion of technology, and the CMS forewarns that requirements will continue to witness changes. The recipe for successfully navigating these changes lies in setting up an integrated framework–people, processes, data and underlying technology–that is efficient and easy to configure for future business requirements.
Clinicians would need to partner with a healthcare IT organization which is not only capable of technology upgrades but demonstrates significant expertise in managing regulatory changes as part of their core business. They will need to acquire specific capabilities that help integrate health information technology and improve collaborations across providers and health systems to succeed in APMs. The right IT partner will need to have extensive capabilities in interoperability, demonstrate regulatory requirement analyses, medical billing, data and process gap analyses, including an extensive portfolio of successful quality reporting to ensure smoother transition to the QPP program.