By Deepak Valecha, Assistant Vice President - Health Plans & Healthcare Consulting, CitiusTech and Prosenjit Dhar, Senior Healthcare Consultant, CitiusTech
Key considerations for a value-based care maturity model – CitiusTech Perspective
Increasingly, payers are shifting population cohorts to an outcome-based, risk-sharing arrangement. To successfully scale the value-based care (VBC) transition, payers must adopt a multi-stage approach. Despite strong willingness, payers and providers struggle to scale value-based care with persistent ROI. Much has already been written on the payer and provider VBC shift. Reassessing the VBC value chain will enable health plans to transition to higher-level maturity VBC models, achieving scalability, greater efficiency, and more sustainable ROI. This article aims to provide a practical perspective on the journey towards steady state VBC and the change management that should be adopted for a smoother transition.
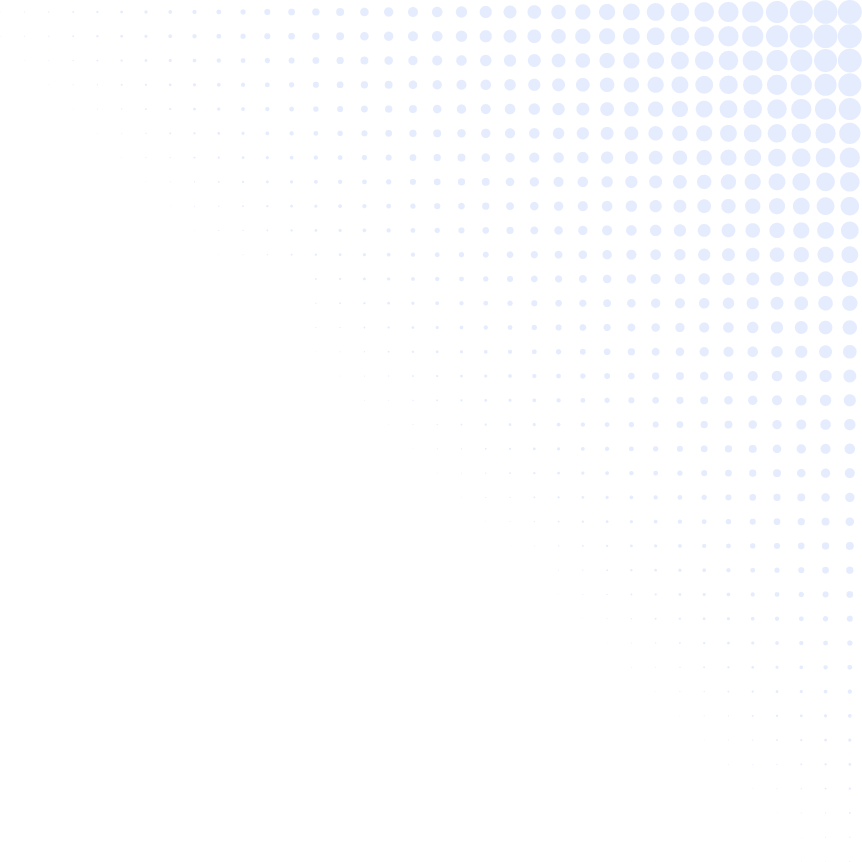
At CitiusTech, based on our engagements with several payers, we have framed a three-level maturity model. Most payers are devising strategies to transition from maturity level 1: incentive payments based on quality reporting Machine Readable File Analytics for Payers
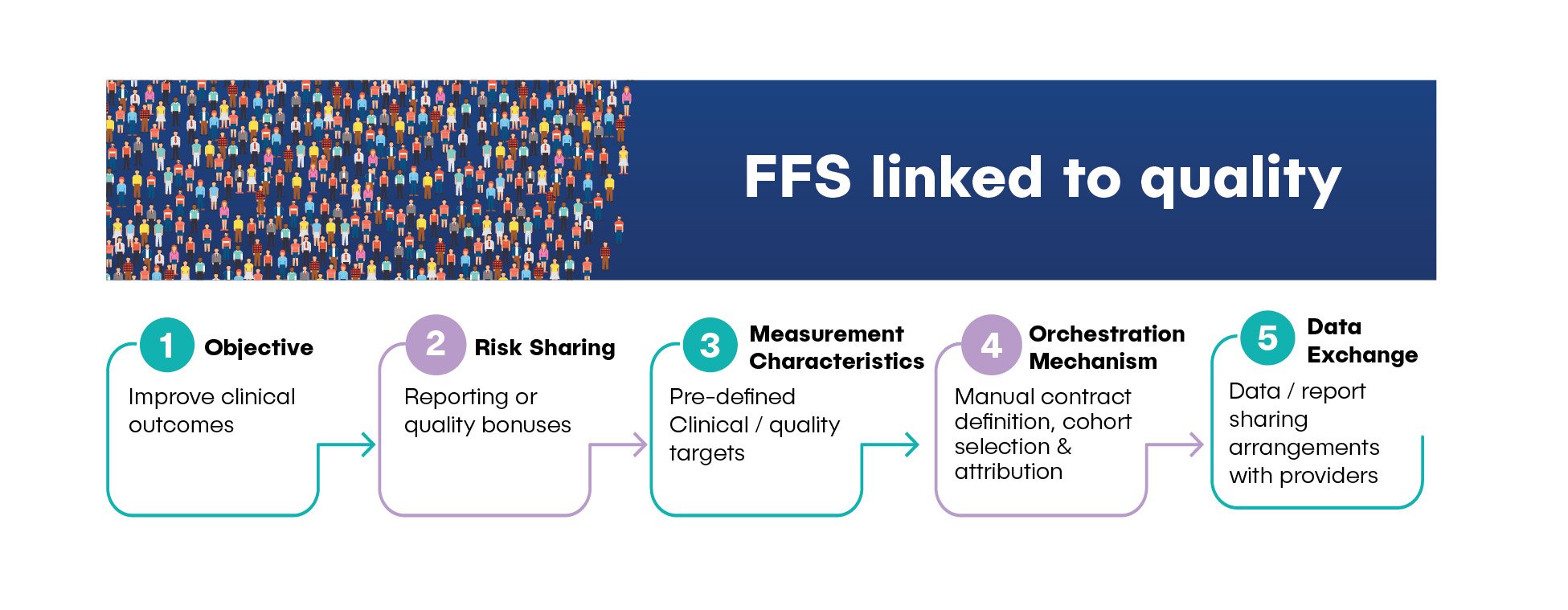 to maturity level 2: single or double-sided risk sharing and incentive payments.
to maturity level 2: single or double-sided risk sharing and incentive payments.
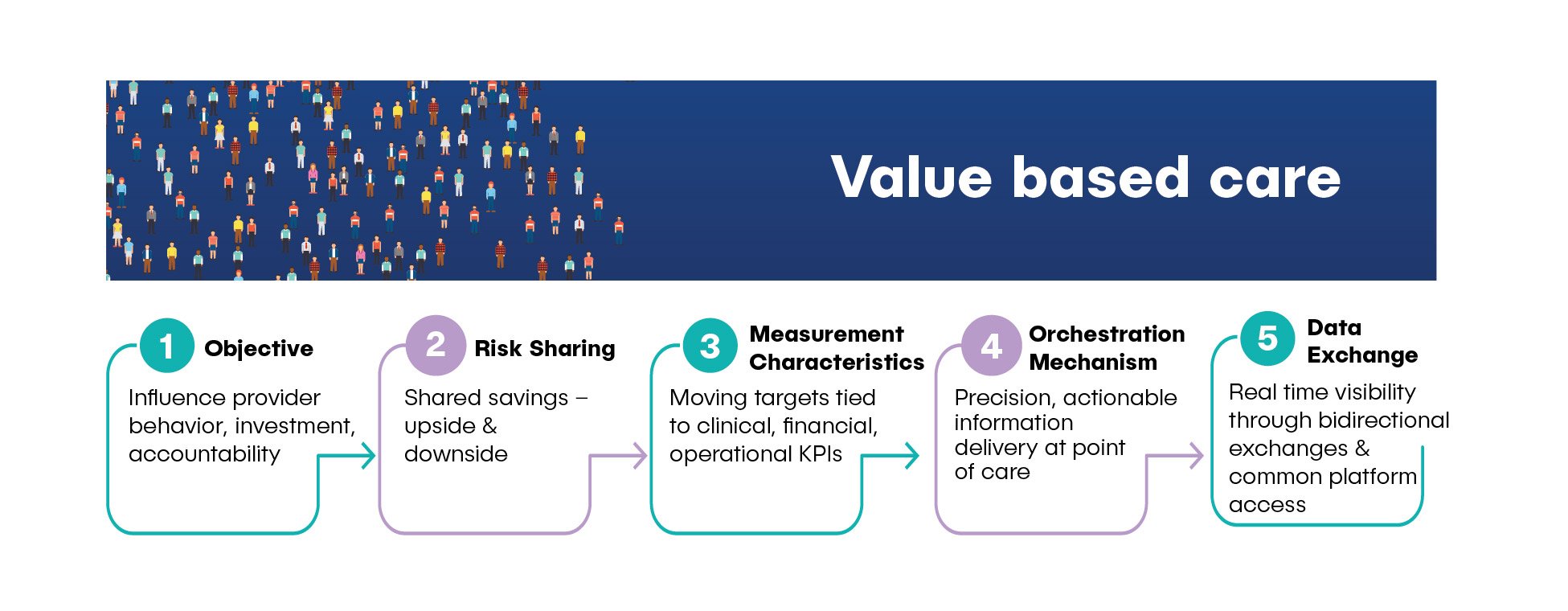 However, with the steady adoption of digital therapeutics and the shift towards care delivery close to home, more health plans are progressing towards maturity level 3: personalized care.
However, with the steady adoption of digital therapeutics and the shift towards care delivery close to home, more health plans are progressing towards maturity level 3: personalized care.
 Matured health plans recognize the need for specialized care for various chronic disease management. Identifying cohorts for specialized care and outsourcing such cohorts to advanced digital therapeutics organizations (e.g. Livongo, Omada Health) through an outcome-based risk arrangement is rising.
Matured health plans recognize the need for specialized care for various chronic disease management. Identifying cohorts for specialized care and outsourcing such cohorts to advanced digital therapeutics organizations (e.g. Livongo, Omada Health) through an outcome-based risk arrangement is rising.
Achieving Personalized Care for Level Three VBC Maturity
The journey from fee-for-service design to personalized care requires a commensurate shift in focus from healthcare service delivery to patient- and member-specific healthcare service alignment. Key goals to achieve steady state VBC maturity would include:
- Strong narrow network orchestration
- Appropriately personalized interventions
- Individual-specific care coordination
- Improved control of cost and quality
- Enhanced appetite for risk sharing
- Incentives to shift towards a larger share of risk in VBC as percentage of PMPM premiums
- Focus on member experience capture and incorporation into incentives
How Interoperability and Patient-Centered Quality Measures Ease VBC Transition
Two industry developments can make the VBC maturity transition easier.
Interoperability Focus: Recent government initiatives by DHHS, CMS, and NCQA, including Digital Quality Measures (DQM), Digital Exchange of Quality Measures (DEQM), and large-scale public-private collaborations (e.g. DaVinci, Gravity, OHDSI), are focusing attention on creating a seamless payer-provider exchange of data.
Patient-Focused Quality of Care Measurements: Keeping patient-centric principles at its core, digital quality and population health analytics are being redesigned to better anchor clinical process, outcome, and experience journeys. This redesign is based on health equity and individual disease progression like Patient Reported Outcomes Measures (PROMs). Together, these measures will continue to move provider organizational focus toward patient-specific health outcomes versus general compliance.
VBC Solutions that Enable Transition to Level 2 and 3 Maturity
Transitioning to Level 2 and Level 3 maturity relies on payers assessing, selecting, and adopting VBC solutions that offer transparency, automation, intelligence, and interoperability. In our view, the critical components for a comprehensive, scalable VBC solution span across the following value chain components:
- Prospecting and modeling: Your ability to test and simulate various value-based arrangements (HCP LAN APM category 3 and 4) against flexible provider selection, cohort selection, metrics selection, and goal configurations while negotiating for optimized value-based goals and incentives that work best for both negotiating parties.
- Contracting agreement: Having a unified system for provider contract management with built-in contracting templates, configurable workflow, team collaboration, document management, and audit capabilities. Contracting systems should further inform the VBC program set-up for onboarded providers.
- Unified VBC system of record: Ensuring capabilities to set up multiple VBC arrangements in a self-guided way. The system should be able to source data from various internal and external payer sources, including claims, clinical, patient-reported health outcomes, social determinants of health, quality, financial, operational, experience, and provider-shared operational data.
- Cost-of-care analytics: Benchmark provider incentives and payments across various variations of VBC arrangements for identifying outliers and opportunities to further optimize, reconcile, or adjust incentives based on prior payments.
- Provider outreach and engagement: Provider training and education to enhance opportunities and access to analytical tools and insights for driving VBC goals.
- Monitoring and performance tracking: Capabilities that enable a single, consolidated scorecard across provider hierarchy, including all associated payer-provider arrangements and book of business. This should also extend transparency analytics to the provider network on VBC goal breakdown, offering further opportunities for optimized earnings.
- Bi-directional engagement and alerts: Integration of real-time alerts and patient information exchange at the care site, driving required actions for gap closure and performance improvement.
- Integrated single-source of provider payments: Integration of VBC incentive calculations and financial system for calculation and release of high-accuracy payments to providers, payment adjustments, and transparent payment reports with granular payment breakdowns.
The value-based program management space is ripe for disruption with payers using a mix of manual efforts, spreadsheet-based tactics, and point solutions. Payers will be well-served to define a long-term VBC technology roadmap that aligns with the maturity curve and balances technology investments over the short- and medium-term.
CitiusTech provides seasoned, global expertise in value-based care contracting, operations, and technology to realize better outcomes and ROI through personalized care. Contact us to discuss the three-level VBC maturity model in more detail.