Authors: Deepak Valecha, Sr. Healthcare Consultant, CitiusTech & Nikita Agrawal, Healthcare Business Analyst, CitiusTech
The COVID-19 pandemic opened the door to one of the biggest humanitarian tragedies in recent memory. The state executive orders mandated hospitals in the US to cancel elective treatments to secure capacity for COVID treatments. The drop in utilization resulted in a significant decline in Medical Loss Ratio (MLR) for payers. At the same time, hospital revenues declined by $323B in FY 20.
Fitch Ratings has revised its ratings for the US health insurance industry from ‘negative’ to ‘stable’ for 2021. As the system recovers, most of the leading health plans have also raised their guidance on the financial outlook. As the number of COVID cases start to decline, healthcare organizations will need to make significant changes in how and where they operate. But the question still remains - whether normalcy is on the horizon for the health insurance industry?
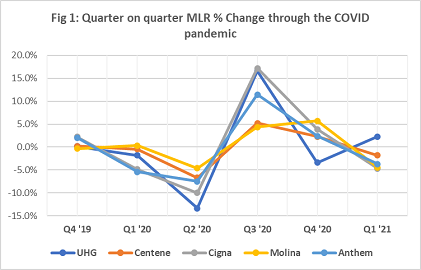
The post pandemic vitals of health insurance industry show (see figure 1) that the MLR has started to improve, given the rise in utilization, compared to the period when the pandemic was at its peak. The comeback is clearly driven by steady fulfillment of delayed electives and other COVID associated outpatient expenditures such as treatment, testing and vaccine administration.
Key factors affecting the health insurance industry
Prominent factors influencing the health insurance industry in the post pandemic world (refer Factors Shaping the Post-COVID Payer Market) are -
- Post-COVID unemployment – Membership shift from commercial to Medicaid
The unemployment rate in the country has been on the rise. As a result, a lot of Americans who lost their employer provided health insurance migrated towards Medicaid. A special enrollment period (SEP) was orchestrated by the federal government where despite the job losses, the enrollment went up to a record high of 528,000 since the start of the SEP. According to a CMS report, consumers signing up for health insurance went up from 171,000 in 2019 to 209,000 in 2020. The new enrollees paid premiums as low as $86 thanks to the premium tax credits. In 2021 OEP (Open Enrollment Period), the percentage of consumers with reported household incomes between 100% and 250% FPL (Federal Poverty Level) increased to 73% as compared to 71% in 2020. Approximately 12 million customers were re-enrolled in the marketplace during the 2021 OEP which indicates a 5% increase from the 2020 OEP.
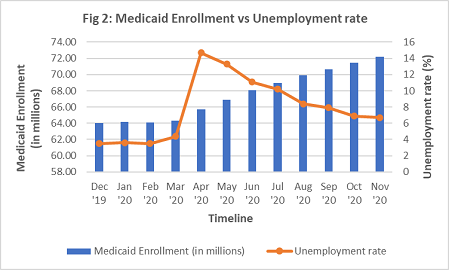
Figure 2 below shows the Medicaid population witnessing an exponential rise despite a decline in unemployment rate. A study said, the consistent rise may be associated with factors other than job loss such as reduced work hours making more people eligible and Medicaid expansion.
- Coverage redesign owing to increased utilization and adverse risk pools
Utilization has increased not just due to elective procedures but also because of COVID related treatments and vaccination drives. The pandemic may be just the first of many battles, because of the long road to recovery for many COVID patients. (“After recovery, patients remain at risk for lung disease, heart disease, frailty, and mental health disorders” a study reports) From this point onwards, revised plan designs, extended benefits and network coverage, all should be looked upon differently by the health plans. Given that businesses are operating with uncertainties, organizations that have a focus on Medicare & Medicaid are likely to be significantly impacted due to the nature of their risk pools. It has now become imperative for such organizations make technology investments to accelerate digital transformation, enable stronger cost optimization and manage their population in an equitable manner.
- Affordability, collaboration and exchange through regulatory push
Emerging regulatory changes could have a significant impact on the business and operating environment for insurers in 2021 and beyond. Affordable telehealth is one of the top priorities for the current US administration. It is just a matter of time before we get to see whether the current flexibilities around telehealth are persisted with or are constrained by tighter regulations. With recent post pandemic guidance from the CMS and other federal/state regulators, changes regarding telehealth accommodation as well as health equity reporting in the HEDIS® quality measures can also be seen. Additionally, the Social Determinants of Health Accelerator Act can also act as a driver for SDOH data sharing & analytics to help better understand member populations.
Way forward: Areas where health plans must go all-in with tech investment
The pandemic has pushed forward the digital transformation agenda for payers by as 5 years at least. As the industry comes to terms with the new normal, it becomes crucial for payers to make significant changes to their business models, powered by next-gen technology. Utilization will be the focus point to drive these changes and payers need to make the right investments today in order to cut costs, reduce risks and generate consumer insights. Some of these investments in the areas of population health, care management and quality improvement also qualify as medical expenses from an MLR calculation standpoint as stated in the Patient Protection & Affordable Care Act.
- Data Integration and Interoperability to deliver Personalized Member Experience
Post COVID, health plans must begin with a focus on data. CMS’ Interoperability rule has kickstarted a journey that will transform clinical, financial and operational data exchanges for the years to come. By identifying data partners and integrating social determinants/device/member reported data elements through real time streaming pipelines, health plans must lay the foundation to improve care delivery and take informed decisions.
- Analytics to React Faster to Business Needs & take Informed Decisions
Health plans must continue investments in traditional and advanced analytics e.g. new data science models that stratify post-pandemic risk scores and project PMPM spend for COVID/non-COVID affected members, can help make better informed financial and underwriting projections. This in return will help closely affected membership teams and product design teams to drive member personalization.
- Digital Architectures to function as Agile Member Centric Enterprises
Health plans must re-evaluate their technology architectures and identify areas of opportunity for modernization. This is a balancing act between leveraging existing investments while also overcoming legacy technology debt. Approaches such as microservices and event-based architectures can drastically speed up information delivery & insights generation across the enterprise through real time analytics.
The next population health exigency might be a few years away, but the right investments, approaches and foresight will ensure that we are better prepared for the future.
Reference Links:
- Health Insurance Profitability During the COVID-19 Pandemic (nih.gov)
- Factors Shaping the Post-COVID Payer Market (managedhealthcareexecutive.com)
- 2021 Marketplace Special Enrollment Period Report | CMS
- HHS: ACA Premiums Drop 25% for New Enrollees on HealthCare.gov (healthpayerintelligence.com)
- 2021 Open Enrollment Report (cms.gov)
- Changes in US Medicaid Enrollment During the COVID-19 Pandemic | Health Care Economics, Insurance, Payment | JAMA Network Open | JAMA Network
- Planning for the Post-COVID Syndrome: How Payers Can Mitigate Long-Term Complications of the Pandemic (nih.gov)
Fig 1: Quarter on quarter MLR % Change through the COVID pandemic
- https://www.unitedhealthgroup.com/investors.html
- https://investors.centene.com/
- https://investors.cigna.com/home/default.aspx
- https://investors.molinahealthcare.com/
- https://ir.antheminc.com/
Fig 2: Medicaid Enrollment vs Unemployment rate