Insights
- Prior authorization plays a crucial role in ensuring that patients receive appropriate and cost-effective care. However, the current manual processes are burdensome for both payers and providers, leading to delays and errors that can impact patient care.
- Electronic prior authorization (ePA) has emerged as a solution to streamline the prior authorization process, offering benefits such as improved efficiency, cost savings, and enhanced provider and patient experiences.
- Despite its benefits, ePA adoption has been sluggish, but recent regulatory changes and the need for operational efficiencies are driving its uptake.
- Payers stand to benefit significantly from implementing ePA, including cost savings, administrative ease, and improved operational metrics. ePA is set to revolutionize prior authorization, offering a faster, more efficient process that improves healthcare delivery and patient outcomes.
The healthcare industry continues to evolve and transform, with heightened patient care serving as the North Star. Though there have been numerous roadblocks along the way, one area that continues to be a hot-button issue is prior authorization. Payers grapple with burdens associated with rising costs, the need for multi-channel maintenance, and burnout. On the other hand, providers’ efficiency, Patient care quality, and delivery are marred by administrative burdens and care delays. In an American Medical Association (AMA) survey, almost 89% of Providers said that prior authorization issues had a negative impact on clinical outcomes.[1]
The importance of the prior authorization process and inherent inefficiencies have garnered immense policy attention over the years. Electronic prior authorization (ePA) has emerged as a solution that can change the narrative and tide over the current challenges in prior authorization.
Challenges with the current Prior Authorization process
The role of prior authorization is to help payers evaluate the necessity of prescribed treatment and approve or deny coverage based on health plan terms before the services are rendered. A prior authorization helps accelerate claim approvals. However, currently, prior authorization relies largely on manual processes involving multiple information exchanges between disconnected teams of Providers and Payers. Additionally, manual decision-making causes inconsistent clinical determinations, leading to denials.[2] This approach to prior authorization is redundant, expensive, time and labor-intensive, and delays necessary patient care as seen below.
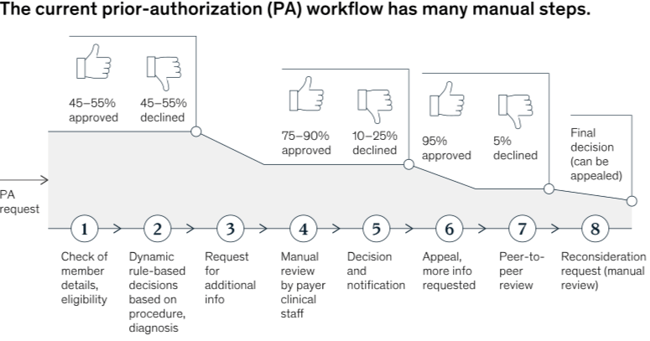
The ‘to-and-fro’ data exchange between the three Ps (Providers, Payers, and Patients) increases timelines, adding strain to the healthcare ecosystem and affecting the ultimate goal: timely and relevant care to ensure better patient outcomes.
Providers find the process opaque and unpredictable[3], making treatment decisions difficult. Keeping track of which services are covered, what coverage has changed, and appealing rejections, etc., takes up a lot of provider time that could otherwise be focused on patient care. Eighty-eight percent of physicians describe the burden associated with prior authorization as high or extremely high, and almost all (94%) of them have reported care delays associated with the process.
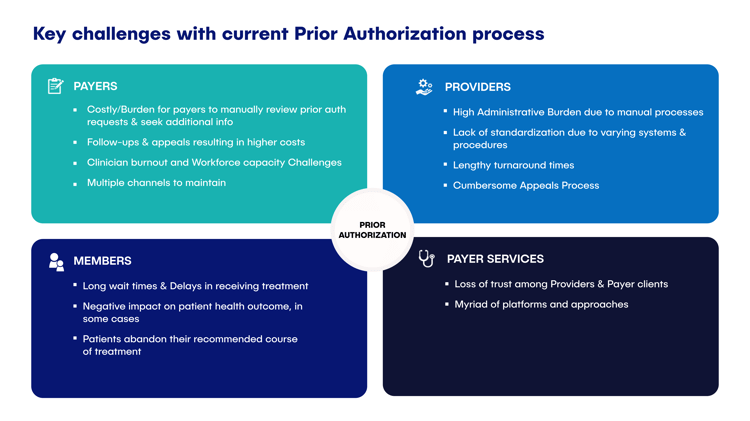 Image 2: Challenge with the current Prior Authorization process
Image 2: Challenge with the current Prior Authorization process
Payers, on the other hand, must go through volumes of documentation and the strenuous administrative tasks of deciphering the medical necessity, prior treatment, clinical indications, and total cost of therapy. The information is fragmented and comes from various sources. For instance, 76% of payers report fax machines and provider portals as primary sources of prior authorization requests.[4] This has brought the whole healthcare ecosystem to a much-needed paradigm shift in the form of Electronic Prior Authorization.
Creating new efficiencies with Electronic Prior Authorization
Electronic prior authorization integrates current workflows by electronically transmitting patient information between providers and payers, improving the drug prior authorization process. Though ePA has been around for a decade, its adoption hasn’t been as agile. According to the Council for Affordable Quality Healthcare’s 2023 CAQH Index, only 31% of prior authorizations are fully electronic.[5]
That is changing now as business realities and regulatory push have created an urgency to embrace ePA. The CMS's final rule[6] on ePA offers Payers a chance to gain a competitive edge in the market. Payers can set a precedent by adopting a much-needed member-centric initiative. The new CMS Rules have the potential to expedite and streamline the process, building member trust and adding business value. In addition to being compliant, ePA offers several strategic advantages to payers:
These use cases represent the potential of democratised cognition to solve many existing healthcare challenges. That said, Generative AI also presents its own share of ethical and technological concerns, such as systemic biases, privacy and confidentiality, the impact of hallucinations, and so on. Here are a few considerations for healthcare organisations to keep in mind as they embark on their Generative AI journey:
- Improved provider and patient experience with fast-tracked processes - Multiple appeals and requests swamp payers. With ePA, Payers can remove unnecessary complexity of the authorization rules, ambiguity, and fact-checking from the equation and expedite processes where they matter. An intelligent, automated prior authorization system can prioritize requests, automate decisions, and accelerate care coordination. Minimizing process delays, multiple requests for documentation, and inappropriate rejections can make a huge difference in the Payer-Provider-Patient equation. The idea is to build trust, enhance member experiences, and stay one step ahead of the competition through real-time ePA processes that speed up responses.
- Administrative ease and cost savings – Follow-ups, appeals, document processing, etc., take up massive administrative bandwidth for Payers. In addition, erroneous approvals could significantly increase the cost of care for the Payers. According to the Council for Affordable Quality Healthcare’s 2023 CAQH Index, the adoption of ePA holds “$494 million in cost savings opportunity annually for the medical industry”.[5] ePA empowers Payers with a standardized and centralized single source of truth, reducing call load where verification and authorizations were requested but not needed. It can reduce administrative work by almost 65%, making time for core administrative processes.[7] Automated workflows reduce manual intervention, streamline the process, improve the accuracy of authorizations, and make it easy to comply with new changes in rules.
- Improve operational metrics & STAR Measure Performance – ePA can improve Star Ratings in multiple ways - enabling rapid access to patient care through automated prior authorization decisions, digitizing the intake process across various channels, and expediting care coordination with interoperability and transparency. Additionally, FHIR-led ePA lays the foundation for improved operational KPIs, such as staff productivity by adopting GenAI that has the potential to streamline prior authorization and claims processing tasks.[8]
Shifting to an efficiency-driven authorization process
Electronic Prior Authorization is the way forward for Payers who want to remain current, improve information exchange timelines, and provide superior member experiences. However, the transition to new processes after investing heavily in the existing systems can be daunting, and the idea of change can seem unsettling. However, a frictionless transition to ePA is a possible reality that can be manifested through existing platforms and investments, causing minimal disruptions in the existing architecture. Payers can change the trajectory of how they gain value from their business with an intelligent mix of new tools and solutions seamlessly integrated with existing technologies. In the next article, we will explore the precise roadmap that Payers can follow in adopting ePA for a smoother transition.
References
- AMA prior authorization (PA) physician survey (ama-assn.org)
- AI ushers in next-gen prior authorization in healthcare (mckinsey.com)
- What doctors wish patients knew about prior authorization (ama-assn.org)
- Prior authorization practice resources (ama-assn.org)
- 2023 CAQH Index Report | A New Normal: How Trends From the Pandemic are Impacting the Future of Healthcare Administration (caqh.org)
- CMS Interoperability and Prior Authorization Final Rule CMS-0057-F (cms.gov)
- 3Q23 Prior Authorization: U.S. Healthcare Payer Perspectives (gartner.com)
- Tackling healthcare’s biggest burdens with generative AI (mckinsey.com)






.png?width=1920&height=1080&name=Consulting2_Menu_1%20(1).png)




























































.webp?width=400&height=400&name=The%20future%20of%20Healthcare%20(1).webp)





















.png?width=400&height=400&name=7-Jun-13-2025-02-27-19-6568-PM%20(1).png)







