By Deepak Valecha, Assistant Vice President - Health Plans & Healthcare Consulting, CitiusTech and Nikita Agrawal, Healthcare Business Analyst, CitiusTech
The COVID-19 pandemic has led to a largescale shift in healthcare industry priorities and membership patterns. In the last few years, health plans significantly altered their financial and operational models to better manage medical loss ratio (MLR), and also made strategic shifts in business – such as M&A, vertical integration and membership mix pivots etc. – to weather the storm.
To assess the ongoing pandemic's impact on the payer landscape, it is critical to understand MLR trends and the change in the membership mix for leading health plans. To achieve this, we compared financial results of Q4 2019 and Q4 2021, using Q4 ’19 as the pre-COVID baseline. We analyzed six leading health plans – United Healthcare, Centene, Cigna, Molina, Anthem, and Aetna – as they represent a large population and are good indicators of business impact.
Our research is a continuation of earlier blogs around health plan business strategy. In 2020, we had anticipated the most prominent factors that would influence the health insurance industry post-pandemic era in our blog “Factors Shaping the post-COVID US Payer market”. Another blog published in 2021, “MLR 2021 Outlook: Is Normalcy on the horizon for Health plans post-pandemic?” emphasized key investment areas for health plans to stay relevant once the pandemic subsides.
- MLRs of leading health plans have normalized to pre-COVID numbers
We analyzed the Medical Loss Ratios (MLRs) of six health plans for the two quarters mentioned above and observed that the MLRs have largely returned to pre-pandemic levels for all the health plans except Molina, owing to net unfavorable COVID-19-related impact (Figures 1 and 2).
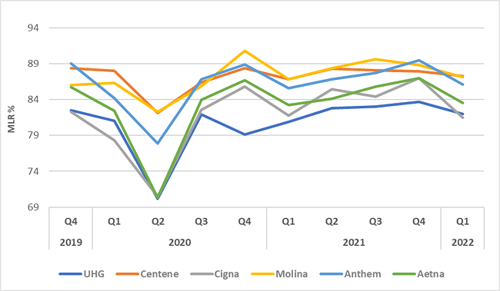
Figure 1: MLR Trends 2019 through 2022
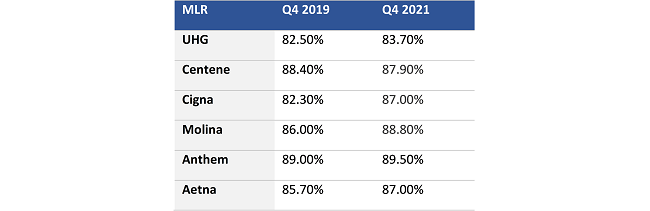
Figure 2: MLR Comparison Q42019 and Q42021
Note: All the observations presented here are for the period from Q4 2019 to Q4 2021 which indicates pre-pandemic vs post-peak pandemic levels.
The recent Q1 22 results (Figure 1) also demonstrate the fact that care patterns are returning to normal. The only major fluctuation from Q4’ 21 to Q1’ 22 is observed in Cigna where MLR is reported at a lower-than-expected rate owing to a drop in COVID testing and treatment costs.
- Membership mix has moved strongly in favor of government plans, which has impacted commercial and ASO membership growth
The MA business grew at 52.6% in these 2 years, where primary gains were made by Aetna and Centene. Medicaid business grew at approximately 49% during the same period (Figure 3). MA growth was considered a strategy shift for health plans focusing on a stable, revenue-assured business line, whereas Medicaid growth was driven by government policies and unemployment spikes. The exception was Cigna which did not focus on Medicaid growth (Figure 3).
Figure 3: Significant increase in Medicaid and Medicare membership during pandemic
(Million members)
MA crossed an important milestone in 2021 – It grew more than any time in its history as 25 million (42% of the 62 million) Medicare enrollees were enrolled into MA. Through the pandemic, Centene pivoted to MA business, through the acquisition of WellCare, which resulted in a 12x growth (Figure 3) in MA revenues. Similarly, Aetna, a subsidiary of CVS Health, expanded its MA business by 67% in 2 years (Figure 3) by offering plans across 1875 counties and extending its reach to 53.2 MA eligible consumers nationwide.
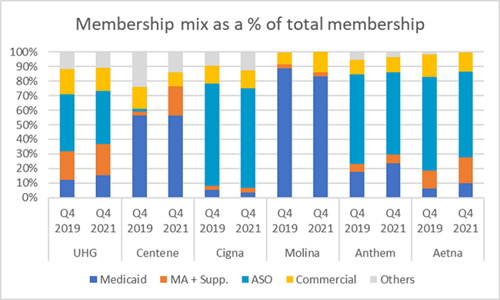
Figure 4: LOB wise membership distribution against total medical membership
Note: Centene includes PDP numbers within Commercial
Overall, most of the health plans analyzed seem to have strategically focused their membership mix towards government businesses. UHG, Anthem, Aetna increased their percentage allocation of both MA and Medicaid membership mix. Centene increased its MA population and decreased reliance on commercial business in its membership mix. Cigna experienced a decrease in its proportionate allocation in MA, Medicaid and ASO due to a decrease in overall US medical membership, increasing its reliance on ancillary & international business. Molina slightly increased allocation in commercial – indicating a potential pivot in its strategy over the coming months.
- Membership mix has moved strongly in favor of government plans, which has impacted commercial and ASO membership growth
The surge in Medicaid business was largely due to pandemic-related unemployment & the government focus on cushioning the blow on the low-income population (Figure 5). The eligibility redeterminations for Medicaid were suspended during the Public Health Emergency (PHE), which led to outsized growth in Medicaid enrollment.
Medicaid enrollment growth was fairly gradual and continues even though unemployment rates have almost normalized to pre-COVID levels, as the PHE remains active as of Apr-Jul 2022. It remains to be seen how the administration prepares for “the great Medicaid unwinding” once the PHE is rolled back later in 2022.
As the pandemic dragged on, the 5 largest companies in the Medicaid managed care market - Centene, UHG, Molina, Aetna, and Anthem emerged as key players whose Medicaid membership scaled up to higher levels (see fig 4). Centene added ~6.5 million Medicaid members aided by the Centene - WellCare merger, Anthem’s expanded its membership in Missouri and Nebraska helping them grow into new geographies.
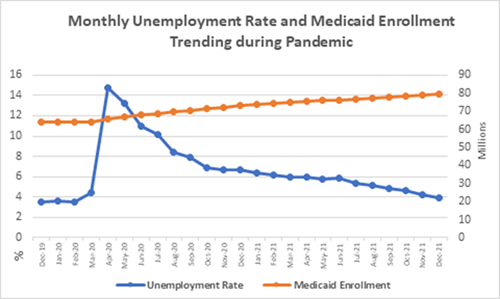
Figure:5: Monthly unemployment rate and Medicaid enrollment trending during pandemic
SOURCE: U.S. Bureau of Labor Statistics, Statista, CMS Medicaid, and CHIP Enrollment Trend
Medicaid growth should eventually slow down as eligibility redeterminations would resume.
Commercial membership enrollment was flat for health plans amidst the pandemic. ASO business saw a minor drop in enrollment due to a reduction in the employment rate. As per a Moody’s report they “expect to see modest growth in the mature commercial sector amid another year of solid economic growth as the US continues to emerge from the pandemic.”
However, recent geo-political events and economic uncertainties have formed another curveball, and related impacts will need to be tracked closely over the next year.
- How Should Payer Respond?
Two years into the pandemic, the unprecedented disruption of the healthcare system presents a unique opportunity for payers to make the most of the newfound momentum for healthcare reform. A significant number of health plans have already operationalized strategies to invest in clinical and care quality improvement solutions as an alternate funding path in case of unexpected MLR drops.
Going forward, large health plans should continue to find ways to optimize MLRs by reducing high drug costs through driving pharmacological innovations, encouraging biosimilar adoption, and going “all-in” for alternate sites of care i.e. virtual-first plans, digital therapeutics investments, and telehealth/ virtual care. Smaller health plans should continue to improve provider performance and reduce costs by investing in narrow network plans and price transparency analytics to stay competitive.
Disclaimer
The analysis provides general information & our perspective and is subject to change as required. All analysis is based on data available in the public domain, and CitiusTech does not own any of the data used. We do not guarantee the accuracy of the statements made or conclusions drawn in this document and we expressly disclaim any warranties or representations such as accuracy, non infringement, third party rights etc.
References
- https://ccf.georgetown.edu/2022/02/11/medicaid-managed-care-financial-results-for-2021-a-big-year-for-the-big-five/
- https://investors.centene.com/financial-info/financial-results
- https://investors.cvshealth.com/investors/events-and-presentations/default.aspx
- https://investors.cigna.com/home/default.aspx
- https://ir.elevancehealth.com/press-releases/
- https://investors.molinahealthcare.com/
- https://www.unitedhealthgroup.com/investors/financial-reports.html
- https://www.healthleadersmedia.com/sites/hlmp/files/files/Moodys%20-%20Health-Insurance-US%20-%2023Feb22_0.pdf